Chronic Foot Moisture
Causes, Solutions, and Prevention

Chronic foot moisture is more than just an uncomfortable inconvenience; it's a gateway to a host of serious foot health problems that can significantly impact your quality of life. From persistent foot odor and embarrassing social situations to painful fungal infections and even more severe complications like cellulitis, excessive foot moisture creates the perfect breeding ground for bacteria and fungi. What many people don't realize is that this seemingly minor issue affects millions of individuals worldwide and can be a symptom of underlying health conditions or simply the result of poor foot care habits. The constant dampness not only makes your feet uncomfortable but also weakens the skin's natural barrier, making you more susceptible to infections, including stubborn toenail fungus that can take months or even years to resolve. Understanding the root causes of chronic foot moisture and implementing effective management strategies is crucial for maintaining optimal foot health and preventing long-term complications that could affect your mobility and overall well-being.
Understanding the Root Causes of Chronic Foot Moisture
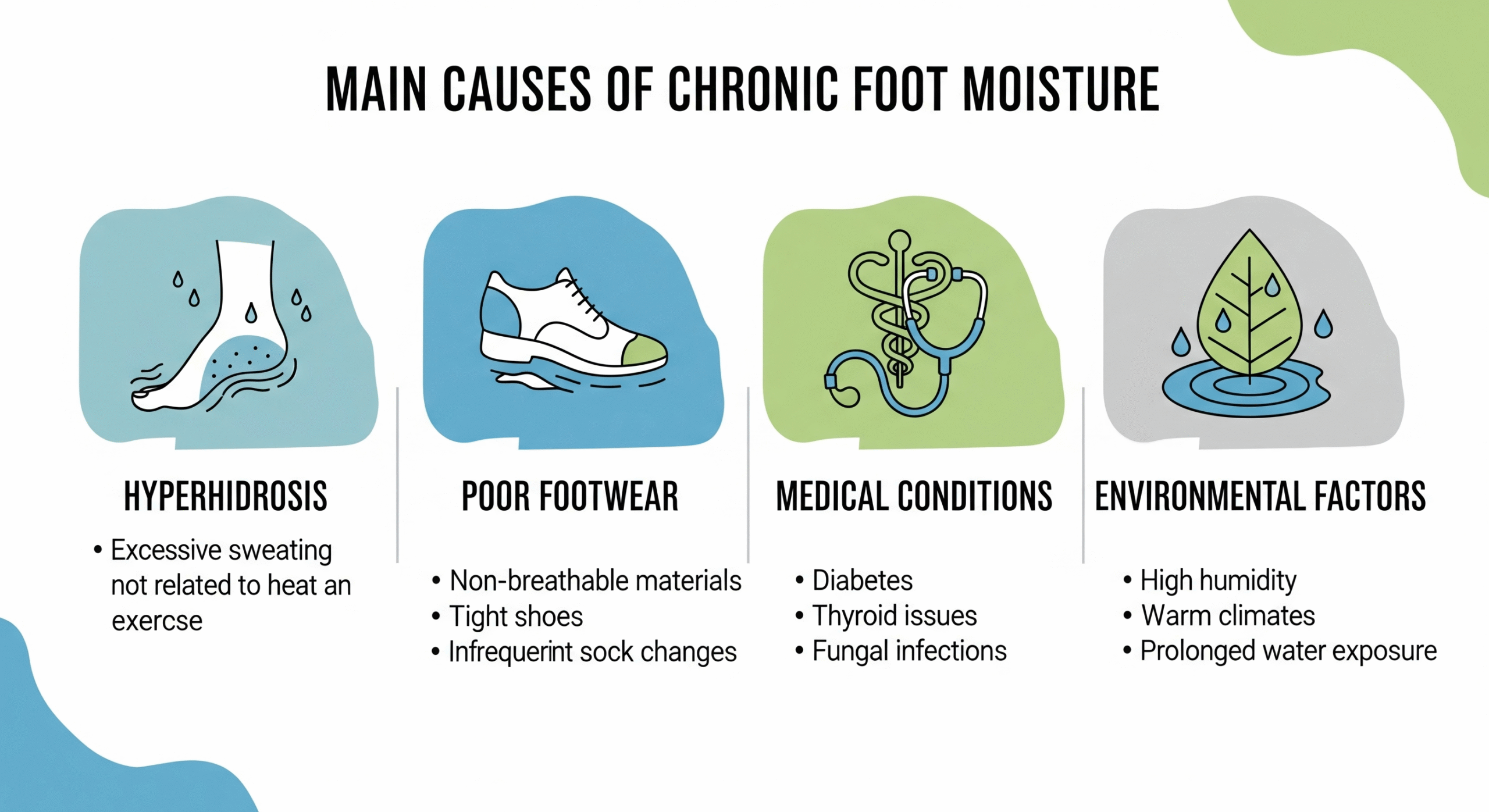
To effectively address chronic foot moisture, it's essential to understand the various factors that contribute to this condition. The causes can range from physiological conditions to lifestyle choices and environmental factors.
Plantar hyperhidrosis is a medical condition characterized by excessive sweating of the feet, often producing more moisture than the body can naturally evaporate. This condition affects approximately 3% of the population and can be either primary (idiopathic) or secondary to other medical conditions. People with hyperhidrosis can produce up to four times the normal amount of sweat, making it nearly impossible to keep feet dry through conventional means alone. The condition often runs in families and typically begins in childhood or adolescence, though it can develop at any age.
Non-breathable shoes made from synthetic materials trap moisture and heat, creating a humid microenvironment around your feet. Tight-fitting shoes compound the problem by reducing air circulation and increasing pressure, which can stimulate sweat production. Additionally, wearing the same pair of shoes daily doesn't allow them to dry out completely, perpetuating the moisture problem. Many athletic shoes, while comfortable, are designed with synthetic materials that prioritize durability over breathability.
Cotton socks, while comfortable, are notorious for retaining moisture against the skin. Unlike synthetic moisture-wicking materials or wool, cotton absorbs sweat and holds it, creating a damp environment that promotes bacterial and fungal growth. Many people unknowingly contribute to their foot moisture problems by choosing socks based on comfort rather than moisture management properties.
Several underlying health conditions can contribute to excessive foot moisture, including diabetes (which can affect circulation and nerve function), thyroid disorders (which can increase overall sweating), obesity (which can increase pressure and heat in the foot area), and certain medications that list increased sweating as a side effect. Hormonal changes during pregnancy, menopause, or puberty can also temporarily increase foot moisture.
Hot, humid climates naturally increase foot moisture, as do occupational environments that require long periods of standing or wearing protective footwear. People who work in kitchens, factories, or outdoor settings often struggle with chronic foot moisture due to environmental conditions beyond their control.
The Hidden Dangers of Chronic Foot Moisture
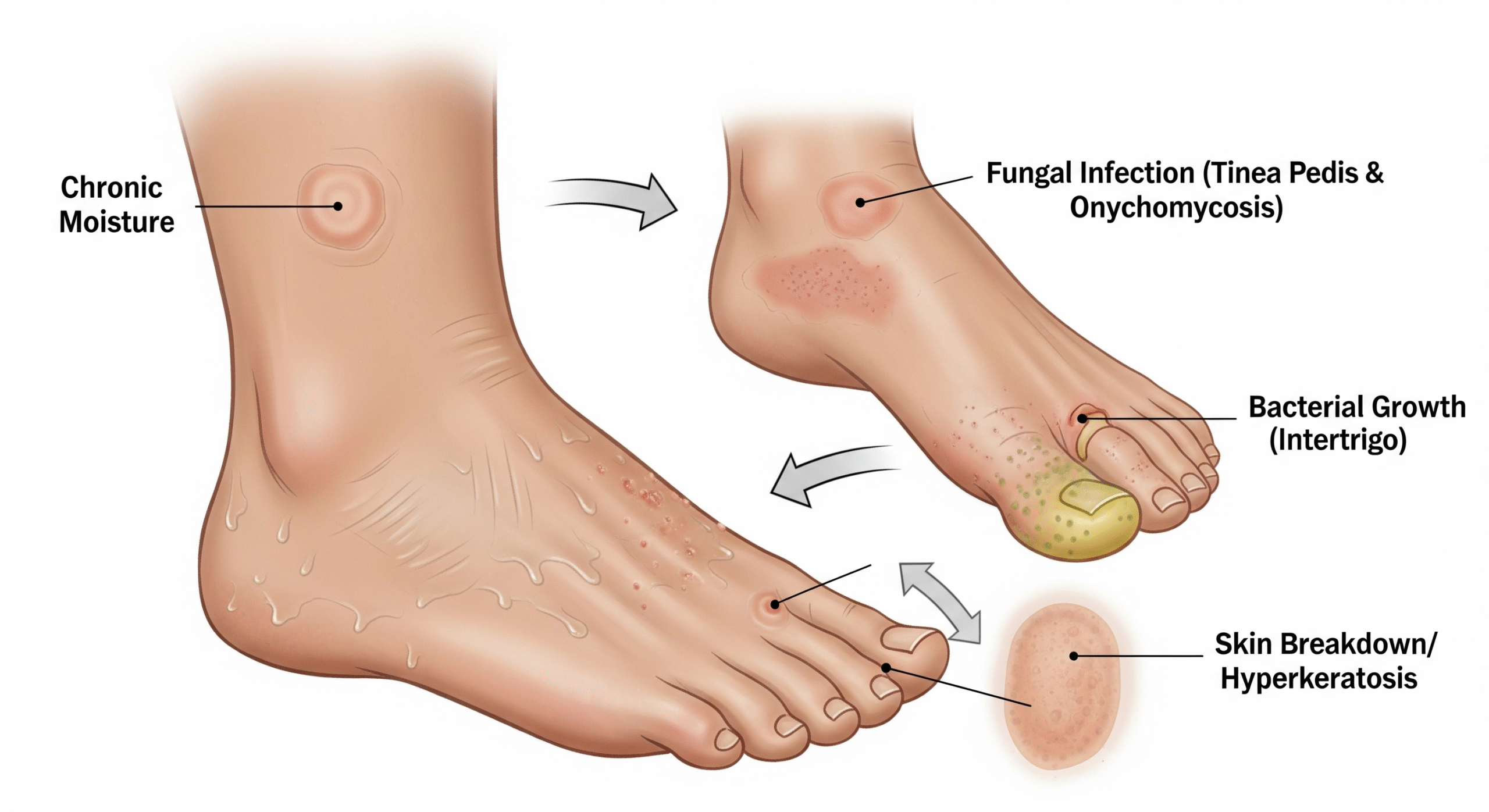
While many people view foot moisture as merely an aesthetic or comfort issue, the reality is far more serious. Chronic moisture creates a cascade of problems that can significantly impact your health and quality of life.
Fungal Infections: The Most Common Complication
Persistent moisture creates an ideal environment for fungal growth, leading to conditions like athlete's foot (tinea pedis) and toenail fungus (onychomycosis). These infections are notoriously difficult to treat and can spread to other parts of the body or to family members. Athlete's foot can cause intense itching, burning, and cracking of the skin, while toenail fungus can lead to thick, discolored, and brittle nails that may require months or years of treatment to resolve completely.
Bacterial Infections and Odor
Bacteria thrive in moist environments, leading to foot odor (bromhidrosis) and potentially more serious bacterial infections. The breakdown of sweat and dead skin cells by bacteria produces the characteristic unpleasant smell associated with sweaty feet. In severe cases, bacterial infections can lead to cellulitis, a serious skin infection that requires immediate medical attention.
Skin Breakdown and Ulceration
Constant moisture weakens the skin's natural barrier function, making it more susceptible to cuts, cracks, and ulcers. This is particularly dangerous for individuals with diabetes or compromised immune systems, as even minor skin breaks can lead to serious infections that may require hospitalization or, in extreme cases, amputation.
Social and Psychological Impact
The embarrassment associated with foot odor and visible fungal infections can lead to social isolation, decreased self-confidence, and avoidance of activities that require removing shoes. This psychological impact can be just as debilitating as the physical symptoms.
Effective Home Solutions for Managing Foot Moisture
While chronic foot moisture can be challenging to manage, there are numerous effective strategies you can implement at home to significantly reduce moisture levels and prevent complications.
Invest in shoes made from breathable materials like leather, canvas, or mesh. Ensure proper fit with adequate toe room to promote air circulation. Most importantly, rotate your shoes daily, allowing each pair at least 24-48 hours to dry completely. Consider using shoe trees or stuffing shoes with newspaper to help them maintain shape and absorb residual moisture. For those with severe moisture problems, having three or more pairs of shoes in rotation can make a significant difference.
Switch to moisture-wicking synthetic materials or merino wool socks that draw sweat away from your skin. Change socks at least once daily, or more frequently if they become damp. Consider carrying an extra pair of socks for mid-day changes, especially during hot weather or periods of increased activity. Some people find that wearing thin liner socks under regular socks can provide an additional moisture barrier.
Wash your feet daily with antibacterial soap, paying special attention to the spaces between your toes. Dry thoroughly, especially between the toes, using a clean towel or even a hairdryer on a cool setting. Apply antifungal powder or cornstarch to absorb excess moisture and create a barrier against fungal growth. Some people benefit from soaking their feet in a dilute vinegar solution (1 part vinegar to 4 parts water) for 10-15 minutes daily to help control bacterial and fungal growth.
Clinical-strength antiperspirants containing aluminum chloride can be effective for reducing foot sweating. Apply to clean, dry feet before bedtime, allowing the product to work overnight when sweat production is naturally lower. Start with every other night to assess tolerance, as some people may experience skin irritation. Over-the-counter options are available, but prescription-strength formulations may be necessary for severe cases.
Use fans or dehumidifiers to reduce ambient humidity in your living space. When possible, go barefoot or wear open-toed shoes to allow your feet to air out. Consider using moisture-absorbing insoles or shoe inserts that can be removed and dried between wears. Cedar shoe inserts not only absorb moisture but also have natural antimicrobial properties.

When Home Remedies Aren't Enough: The Role of Targeted Supplements
While the home strategies outlined above are essential for managing chronic foot moisture, sometimes they're not sufficient, especially when dealing with persistent fungal infections or when your body's natural defenses need additional support. This is where high-quality, targeted supplements can provide a significant advantage, working from within to strengthen your body's ability to fight off moisture-related complications.
Consider this: topical treatments for fungal infections often struggle to penetrate deeply enough to reach the root of the problem, especially in cases of toenail fungus where the infection is embedded within the nail bed. Prescription medications can be effective but may come with unwanted side effects or contraindications. Targeted supplements, however, provide your body with concentrated doses of powerful antifungal compounds and immune-supporting nutrients that work systemically to combat infections, strengthen your natural defenses, and promote healthy skin and nail integrity.
The beauty of a supplement-based approach is its convenience and comprehensive action. Instead of juggling multiple topical treatments, dealing with messy applications, or worrying about remembering to apply products throughout the day, you can support your body's natural healing processes with a simple daily routine. This approach is particularly valuable for busy individuals who want effective results without the time-consuming maintenance that topical treatments often require.
Key Ingredients in Effective Anti-Fungal Supplements:
- Undecylenic Acid: A powerful fatty acid with proven antifungal properties that works systemically to combat fungal overgrowth.
- Caprylic Acid: A medium-chain fatty acid that disrupts fungal cell membranes and inhibits growth.
- Oregano Oil Extract: Contains carvacrol and thymol, compounds with potent antifungal and antibacterial properties.
- Garlic Extract: Rich in allicin, a sulfur compound with broad-spectrum antimicrobial activity.
- Probiotics: Support a healthy gut microbiome, which is crucial for maintaining strong immune function and preventing fungal overgrowth.
- Zinc: Essential for immune function and skin health, helping to maintain the integrity of the skin barrier.
- Vitamin C: A powerful antioxidant that supports immune function and collagen production for healthy skin.
- Biotin: Supports healthy nail growth and strength, crucial for preventing fungal penetration.
🚀 Break Free from Chronic Foot Moisture!
Don't let persistent foot moisture control your life. While good hygiene and proper footwear are essential, targeted supplements can provide the internal support your body needs to effectively combat fungal infections, strengthen your natural defenses, and maintain healthy, dry feet. Save time and money on endless topical treatments and invest in a solution that works from the inside out.
Discover Top Fungus Supplements →Scientifically-backed formulations for lasting results
Advanced Strategies for Severe Cases
For individuals with severe chronic foot moisture that doesn't respond to basic interventions, more advanced strategies may be necessary.
Prevention: Your Best Defense
The most effective approach to managing chronic foot moisture is prevention. By implementing consistent preventive measures, you can often avoid the complications associated with excessive foot moisture.

When to Seek Professional Help
While many cases of chronic foot moisture can be managed with home strategies and supplements, certain situations require professional medical attention:
- Persistent fungal infections that don't respond to over-the-counter treatments
- Signs of bacterial infection (increased redness, warmth, pus, red streaking)
- Skin breakdown, ulcers, or non-healing wounds
- Severe hyperhidrosis that significantly impacts quality of life
- Underlying medical conditions like diabetes that complicate foot care
- Sudden changes in foot moisture patterns that might indicate underlying health issues
Frequently Asked Questions
💡 Take Control of Your Foot Health Today!
You now have the knowledge to effectively manage chronic foot moisture and prevent its complications. For those persistent issues or to give your body an extra edge in fighting off moisture-related infections, remember that targeted supplements can provide the internal support you need for lasting results.
Get Your Foot Health Solution →Invest in dry, healthy, confident feet
Scientific References
- International Hyperhidrosis Society. (n.d.). Plantar Hyperhidrosis. Retrieved from https://www.sweathelp.org/hyperhidrosis-treatments/plantar-hyperhidrosis.html
- Mayo Clinic. (2023). Hyperhidrosis (excessive sweating). Retrieved from https://www.mayoclinic.org/diseases-conditions/hyperhidrosis/symptoms-causes/syc-20367152
- American Academy of Dermatology Association. (n.d.). Athlete's foot: Overview. Retrieved from https://www.aad.org/public/diseases/a-z/athletes-foot-overview
- Strutton, D. R., Kowalski, J. W., Glaser, D. A., & Stang, P. E. (2004). US prevalence of hyperhidrosis and impact on individuals with axillary hyperhidrosis: Results from a national survey. Journal of the American Academy of Dermatology, 51(2), 241-248.
- Haider, A., & Shaw, J. C. (2004). Treatment of acne vulgaris. JAMA, 292(6), 726-735.
- Ghannoum, M. A., & Isham, N. (2014). Fungal nail infections (onychomycosis): A review. Journal of the American Academy of Dermatology, 71(5), 937-951.
- Elewski, B. E. (1998). Onychomycosis: Pathogenesis, diagnosis, and management. Clinical Microbiology Reviews, 11(3), 415-429.
- Walling, H. W. (2009). Primary hyperhidrosis increases the risk of cutaneous infection: A case-control study of 387 patients. Journal of the American Academy of Dermatology, 61(2), 242-246.
- Solish, N., Bertucci, V., Dansereau, A., Hong, H. C., Lynde, C., Lupin, M., ... & Vender, R. (2007). A comprehensive approach to the recognition, diagnosis, and severity-based treatment of focal hyperhidrosis: Recommendations of the Canadian Hyperhidrosis Advisory Committee. Dermatologic Surgery, 33(8), 908-923.
- Hoorens, I., & Ongenae, K. (2012). Primary focal hyperhidrosis: Current treatment options and a step-by-step approach. Journal of the European Academy of Dermatology and Venereology, 26(1), 1-8.

Wagner P
Natural Health Researcher & Founder of LabOfficial
Wagner is dedicated to researching and testing safe, natural solutions for everyday health problems. Through LabOfficial, he shares effective home remedies and recommends science-backed supplements that simplify healing and restore well-being without side effects.
Disclaimer: The information contained in this article is for educational and informational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of a qualified health professional before starting any new diet, exercise program, or supplementation.